|
Resumen
Video resumen del artículo |
INTRODUCCIÓN
Durante las últimas décadas la epidemia de obesidad y diabetes tipo 2 (DT2) aumentó tanto que se ha convertido en una de los desafíos para la salud más importantes en todo el mundo debido a la morbimortalidad y la disminución de la calidad de vida relacionada con esta epidemia. A pesar de todos los esfuerzos preventivos la frecuencia de estas dos entidades continúa creciendo exponencialmente. Un estudio proyectó que para 2050 hasta un tercio de la población de los EE. UU y probablemente también de la población mundial padecerá DT2 [1]
La respuesta biológica subnormal de los tejidos a concentraciones normales de insulina se denomina resistencia a la insulina (es decir, el cuerpo produce insulina, habitualmente en concentraciones mayores que en sujetos normales, pero no la emplea eficazmente) [2].
Este es uno de los factores fisiopatológicos clave de la DT2 y suele aparecer años antes del diagnóstico clínico de diabetes. Se sugirió que la resistencia a la insulina se produce por el exceso de tejido adiposo (obesidad), que tiene efectos bioquímicos debidos a la secreción de múltiples citocinas [MCP-1, TNF-a, IL-6, IL-18, leptina, resistina, e inhibidor del activador de plasminógeno (PAI)-1, entre otros], que se traducen clínicamente como síndrome metabólico [3].
El pinzamiento euglucémico es una técnica compleja que se considera el método de referencia para el diagnóstico de resistencia a la insulina [4].
Dada la complejidad inherente de esta prueba, su costo y la falta de implementación en la práctica médica habitual, hay varias pruebas indirectas para evaluar la resistencia a la insulina, entre ellas: el aumento de la glucemia en ayunas, la relación triglicéridos/ lipoproteínas de alta densidad y la concentración de insulina en ayunas. A fin de evaluar la resistencia a la insulina, estas mediciones se emplearon para crear índices como el modelo homeostático de evaluación de la resistencia a la insulina (HOMA-IR, por las siglas del inglés) y el índice de verificación cuantitativa de sensibilidad a la insulina (QUICKI) [4].
No obstante, ninguna de estas pruebas es suficientemente fiable y por lo tanto no se recomiendan. La observación de las manifestaciones cutáneas de resistencia a la insulina, en cambio, es fiable y coincide con los resultados de la prueba de pinzamiento euglucémico [5, 6].
Además, tiene ciertas ventajas importantes: se observan durante el examen físico, no son invasivas, no llevan tiempo, no son molestas ni significan aumento de los costos. Este artículo intenta ayudar a los médicos generalistas, los médicos de familia y los dermatólogos a reconocer las manifestaciones cutáneas de la resistencia a la insulina. Esto puede poner de manifiesto qué pacientes están en riesgo de sufrir DT2, generando la evaluación adecuada y, de ser necesario el tratamiento oportuno. Se podría así contribuir a evitar la carga de diabetes/síndrome metabólico y aumentar la calidad de la atención para estos pacientes
► La resistencia a la insulina y su asociación con manifestaciones cutáneas
La resistencia a la insulina se define como la disminución de la respuesta de una célula o un órgano a la concentración de insulina a la que está expuesto
La insulina es una hormona peptídica sintetizada y segregada por las células beta del páncreas. La glucosa es el principal regulador de la secreción de insulina; a medida que la concentración de glucosa aumenta, estimula la secreción de insulina. Algunos de los efectos glucorreguladores de la insulina son la inhibición de la glucogenólisis y la gluconeogénesis, el aumento de transporte de la glucosa al tejido adiposo y al músculo, la estimulación de la síntesis de glucógeno, así como su importancia central en el metabolismo de lípidos y proteínas [2, 7].
Como ya se mencionó, la resistencia a la insulina se define como la disminución de la respuesta de una célula o un órgano a la concentración de insulina a la que está expuesto: en la práctica, se refiere al estado en el que la secreción de insulina se asocia con una respuesta anormal de la glucosa (por ejemplo, intolerancia a la glucosa o diabetes) [8].
|
Existen cuatro tipos de la resistencia a la insulina: tipos A, B, C y causas secundarias.
|
Alrededor del 50% de los pacientes con resistencia a la insulina, a pesar de la hiperinsulinemia compensatoria, tienen cierto grado de hiperglucemia ([100 mg/dl). Sin embargo, no todos los pacientes con hiperinsulinemia y resistencia a la insulina tendrán intolerancia a la glucosa o diabetes. Es importante reconocer que prácticamente todo paciente con DT2 tendrá resistencia a la insulina años -o por lo menos meses- antes del diagnóstico de diabetes. La resistencia a la insulina se puede presentar con un amplio espectro de manifestaciones, tales como:
|
Esta asociación se produce porque la hiperinsulinemia activa directa e indirectamente los receptores del factor 1 de crecimiento insulínico (IGF-1) ubicado en los fibroblastos y los queratinocitos, estimulando su proliferación [11, 12].
La hiperinsulinemia también puede influir sobre la producción de esteroides sexuales. Asimismo, la insulina y el IGF-1 aumentan los andrógenos ováricos. Es importante mencionar que enfermedades de la piel como:
- psoriasis
- hidradenitis supurativa
- vitiligo
Se han asociado fuertemente con resistencia a la insulina y síndrome metabólico [4].
► Importancia de la obesidad y la DT2
La prevalencia de obesidad y la DT2 continúa en aumento a pesar de numerosos esfuerzos y ambas parecen imparables. En 2014, más de 1900 millones de adultos tenían sobrepeso y más de 600 millones eran obesos. Al mismo tiempo, más de 380 millones de personas en el mundo padecen diabetes y el 35–50% de la población mundial (>3000 millones) tiene gran riesgo de padecerla—la llamada prediabetes, que en todos los casos se acompaña de resistencia a la insulina.
El impacto de estas dos entidades no es solo por la carga de enfermedad, sino más por el aumento del riesgo cardiovascular, los trastornos musculoesqueléticos, el costo, la mortalidad, la carga del tratamiento y la disminución de la calidad de vida asociados. Ambas entidades sufren la influencia de factores genéticos, epigenéticos y ambientales. Entre estos últimos están el sedentarismo, las comidas poco saludables y el bajo nivel socioeconómico, entre otros [10].
La obesidad se considera la enfermedad concomitante y el factor de riesgo más frecuente para la diabetes, ya que el 80% de los pacientes con diabetes tienen sobrepeso o son obesos. El 70–80% de los pacientes con obesidad tendrán resistencia a la insulina. La obesidad y la DT2 se asocian con una cantidad considerable de dermatosis, entre ellas acantosis pigmentaria, acrocordones, hirsutismo y queratosis pilaris [10].
Alrededor de un tercio de los pacientes con diabetes tendrán algún tipo de manifestación cutánea durante el curso de su enfermedad [13]. Un estudio reciente publicó que el 91% de los pacientes con diabetes tienen por lo menos una manifestación dermatológica [13]. De ahí que todos estos trastornos cutáneos deben alertar a los médicos para estudiar las características metabólicas de estas personas, lo que puede generar un rápido diagnóstico.
► Manifestaciones cutáneas de resistencia a la insulina
♦ Acrocordones
Los acrocordones, también llamados pólipos fibroepiteliales, papilomas cutáneos o fibromas blandos, son uno de los tumores cutáneos más frecuentes [14]. Son benignos, raros antes de los 30 años, pero muy comunes después, especialmente en la ancianidad. Son más frecuentes entre las mujeres y en los pacientes con sobrepeso u obesidad, aunque también tienen una relación familiar/genética. Recientemente, varios estudios asociaron los acrocordones con la intolerancia a la glucosa y la diabetes [15–18].
En 1976, Margolis et al, efectuaron uno de los primeros estudios y publicaron que el 9,4% de 500 pacientes hospitalizados tenían acrocordones y de ellos, el 72% padecían DT2 y sugirió que los acrocordones podrían ser un factor de riesgo para la diabetes [19]. A fines de la década de 1980, Norris et a, informaron una relación entre los papilomas cutáneos y la resistencia a la insulina (el 61% de la población que estudiaron tenía hiperinsulinemia). Sin embargo, sólo el 15% tenía también aumento de la glucemia en ayunas. El estudio de Kahana et al, revelaron que el 34% de los pacientes con acrocordones padecía DT2 [20].
La insulina es una hormona promotora del crecimiento. La hiperinsulinemia se ha vinculado directamente con el IFG-1 y la disminución de la proteína 3 de unión al factor de crecimiento tipo insulina (IGFBP-3). El IGF-1 se une a los receptores de los queratocitos, desencadenando la hiperplasia epidérmica, y la reducción de la IGFBP-3 puede disminuir la transcripción de los genes antiproliferativos activados normalmente. Estas perturbaciones endócrinas alteran la proliferación celular y a la larga se hacen evidentes como papilomas cutáneos [12].
Estas lesiones son tumores pequeños, blandos, levemente hiperpigmentados de tamaño variable y característicamente pediculados (véase Fig. 1). Los acrocordones con frecuencia son múltiples, pero pueden parecer una lesión única. Aparecen con más frecuencia en las zonas intertriginosas, como cuello, axilas e ingles, aunque también se las puede hallar en párpados y pliegues inframamarios [16, 18, 21]. Estas lesiones cutáneas son totalmente asintomáticas, pero pueden ser dolorosas cuando se irritan [22]. El diagnóstico diferencial es con los nevus melanocíticos, los neurofibromas y la queratosis seborreica pediculada.
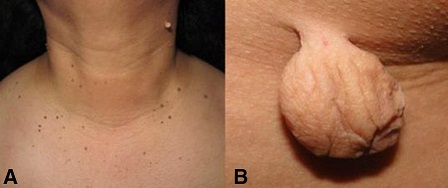
Figura 1. A. Presentación típica de acrocordones mostrando multiples tumors pequeños pedunculados. B. Acrocordon gigante, blando y pedunculado. Elaborado sobre el contenido del artículo de González-Saldivar.
Las enfermedades con las que se asocian son el síndrome de Gardner, el síndrome de Birt-Hogg-Dube y la esclerosis tuberosa, entre otras [18, 23]. El diagnóstico es clínico; si bien puede haber casos atípicos en los que la extirpación quirúrgica y la histopatología confirmarán el diagnóstico. El tratamiento es más una preocupación estética que médica. Los métodos más empleados son la electrocirugía y la crioterapia, aunque el problema con esta última es la dificultad para limitar la zona a congelar exclusivamente a la lesión [25]. Lo más sencillo es extirpar el papiloma con una tijera afilada de buena calidad.
♦ Acantosis pigmentaria (o nigricans).
La acantosis pigmentaria (AP) se caracteriza por placas simétricas, aterciopeladas, hiperpigmentadas, especialmente en las zonas intertriginosas: cuello, axilas y codos, (véase Fig. 2, [5, 9, 26, 33, 36] aunque también pueden estar en otros sitios.

Figura 2. Acantosis nigricans. Elaborado sobre el contenido del artículo de González-Saldivar.
Habitualmente se relaciona con trastornos asociados con resistencia a la insulina (por ej DT2 y obesidad). En casos raros puede aparecer como signo de un tumor maligno (por ej, adenocarcinomas agresivos del tubo digestivo) [26–28]. La AP se clasifica según su etiología en ocho tipos: benigno, asociado con la obesidad, sindrómico, maligno, distal, unilateral, inducido por fármacos y mixto [26].
El ácido nicotínico es el medicamento que causa AP con mayor frecuencia, aunque no el único
La AP asociada con la obesidad, también llamada ‘‘pseudo-AP’’, es la causa más frecuente de AP y es una expresión de resistencia a la insulina. La AP sindrómica comprende los síndromes de resistencia a la insulina tipo A y B (por ej síndrome de Berardinelli-Seip, síndrome de Lawrence), síndrome de Crouzon y otros numerosos trastornos sindrómicos raros. La AP maligna se asocia con adenocarcinomas del tubo digestivo; es grave, abrupta, exuberante y afecta las membranas mucosas.
El ácido nicotínico es el medicamento que causa AP con mayor frecuencia, aunque no el único. En estos casos la AP desaparece espontáneamente en 4–11 meses después de suspender la medicación [26]. Los datos sobre la verdadera frecuencia de la AP son contradictorios, ya que varía mucho según la edad, la etnia, el fototipo cutáneo y las características antropométricas [32–34]. Un estudio con 675 adolescentes halló una prevalencia de AP del 18,9%.
La prevalencia de AP fue mayor en estudiantes obesos que en aquellos con IMC normal (49,2% vs. 7,7%) [6]. Un estudio con 703 estudiantes latinos halló una prevalencia de AP del 47,8% [32]. Además, se encontró AP en alrededor del 50% de los pacientes con síndrome de Down, que también son proclives a la obesidad, el síndrome metabólico y la diabetes [35]. La patogenia es similar a la de los acrocordones y se produce por estimulación del factor de crecimiento de los queratinocitos y los fibroblastos en la dermis.
La familia del receptor de tirosina cinasa comprende la insulina, el IGF, el factor de crecimiento epidérmico y los receptores del factor de crecimiento de los fibroblastos, entre otros. El aumento de la concentración de insulina se traduce en la proliferación de queratinocitos y fibroblastos debido a la estimulación de los receptores del IGF-1 [9, 11, 26].
Además de los lugares anteriormente mencionados un estudio de los autores de este artículo reveló que la ubicación más frecuente de AP, incluso en sujetos con IMC normal fue en los nudillos [32]. Los cambios histopatológicos son sutiles y consisten en hiperqueratosis, acantosis y papilomatosis leve. El color amarronado de esta dermatosis se debe al engrosamiento del estrato córneo. El primer paso en la evaluación de la AP es determinar su etiología.
La información importante comprende:
- la edad
- el momento de inicio
- la evolución
- las mediciones antropométricas
- los antecedentes familiares del síndrome metabólico
- las medicaciones y los datos relacionados con el síndrome diabético (por ej , poliuria, polidipsia, polifagia, adelgazamiento)
- síntomas sugestivos de tumor maligno
En todos los pacientes con sobrepeso u obesidad se recomienda la pesquisa de hiperglucemia en ayunas y pruebas de función hepática.
Para la mayoría de los casos (AP inducida por obesidad), se debe recomendar descenso de peso y ejercicio como tratamiento de primera línea [26, 39]. Otros autores comunicaron el empleo de retinoides orales o tópicos (que probablemente regulen la proliferación y la diferenciación de los queratinocitos) como tratamientos eficaces [26, 40, 41]. También se emplean tratamientos locales con acitretina, lactato de amonio, ácido láctico, exfoliación con ácido tricloroacético, con respuesta variable [39, 43].
♦ Alopecia androgénica
La alopecia androgénica (AAG) es el subtipo más frecuente de alopecia no cicatrizal. La AAG es un rasgo físico hereditario andrógenodependiente, producido por la conversión de los pelos terminales del cuero cabelludo en vellos diminutos con un patrón característico [44]. Afecta a hombres y mujeres en las mismas proporciones y habitualmente aparece al término de la adolescencia [45–47]. Al llegar a los 30 años casi un tercio de los hombres tendrán AAG. Esta proporción aumenta con la edad (alrededor del 50% a los 50 años) [48].
El riesgo de tener AAG depende de varios factores, entre ellos los antecedentes familiares y factores genéticos. Otros factores relacionados son el tabaquismo, la hiperplasia prostática benigna y el cáncer de próstata. Paradójicamente, uno de los factores más frecuentes fue mencionado recién hace poco tiempo—el síndrome metabólico (es decir, la resistencia a la insulina) [45, 48]. Recientemente, Nabaie et al, comunicaron una relación no significativa entre la alopecia androgénica y la resistencia a la insulina en un estudio de casos y controles; sin embargo otros argumentaron que la alopecia androgénica temprana es un marcador de resistencia a la insulina [49, 50].
La dihidrotestosterona (DHT) es el andrógeno implicado en la patogénesis de la AAG. La testosterona se metaboliza en muchos tejidos de la piel; penetra en la membrana celular y es convertida por la 5-alfa reductasa del citoplasma en su forma más potente: la DHT. La 5-alfa reductasa tiene dos isotipos [44, 52]. El tipo II domina en la vaina externa de los folículos pilosos del cuero cabelludo, la barba y el tórax [44]. La DHT se une a los receptores del andrógeno y es transferida al núcleo, donde estimula la transcripción de genes. Esta activación es clave, ya que es la responsable de la transformación gradual de los folículos terminales en pelos vellosos más pequeños [51, 53].
En un estudio de casos y controles en hombres jóvenes con AAG y sin ella, González-González et al, evaluaron diferentes mediciones de resistencia a la insulina en esta población. El índice HOMA-IR y la testosterona libres fueron significativamente más altos en los casos que en los controles [45]. Bakry et al, estudiaron a 100 varones con AAG y sugirieron que a los pacientes en etapa III o mayor se los debería evaluar para síndrome metabólico y resistencia a la insulina [54]. Una revisión sistemática más reciente, que incluyó 31 estudios y 50956 personas (29254 con AAG), reveló que estos pacientes tenían aumento del riesgo de enfermedad coronaria, hipertensión, resistencia a la insulina y dislipidemia [55]. La calvicie en los hombres con AAG suele comenzar con retroceso bitemporal del nacimiento del pelo, así como adelgazamiento difuso del pelo en la coronilla (véase Fig. 3).

Figura 3. Alopecía. Elaborado sobre el contenido del artículo de González-Saldivar.
Más tarde, la pérdida total del pelo centralmente en la coronilla produce un parche de calvicie que se expande gradualmente, uniéndose al retroceso del nacimiento del pelo. La pérdida del pelo habitualmente comienza después de la pubertad [56]. Este tipo de alopecia suele ser progresivo, simétrico y asintomático. En las mujeres la AAG típicamente comienza con la disminución difusa de la densidad capilar sobre las zonas frontal y central, aunque las zonas parietal y occipital también pueden estar afectadas [46] (véase Fig. 3).
La anamnesis debe incluir la edad, el sexo, la existencia de tabaquismo, la evolución de la pérdida de pelo, los antecedentes familiares, los síntomas asociados, los tratamientos previos y el empleo de medicamentos (por ejemplo esteroides anabólicos). En las mujeres se debe efectuar una anamnesis ginecológica detallada que incluya menarca, ciclo menstrual, amenorrea, menopausia, empleo de tratamiento hormonal, trastornos de la fecundidad y signos de hiperandrogenismo.
El examen dermatológico debe incluir, además del cuero cabelludo, la distribución capilar en el cuerpo, piel y uñas [46]. El cuero cabelludo suele ser normal, pero es común hallar dermatitis seborreica. En pacientes con AAG el examen físico total es especialmente importante, ya que está muy asociado con otras enfermedades, como la enfermedad coronaria y el síndrome metabólico [45, 47, 48, 54, 55, 57].
La prueba de pilotracción se debe efectuar siempre en las zonas parietal derecha e izquierda, frontal y occipital, así como en la zonas afectadas. Esta prueba solo es positiva en sujetos en la fase activa de la AAG. Según el contexto, se puede considerar la medición de la tirotropina, el hierro y los andrógenos, a fin de descartar otras causas de [47]. La dermatoscopia es útil para el diagnóstico de AAG. El signo dermatoscópico clásico es la diferencia mayor del 20% del diámetro del pelo (anisotricosis) con los pelos vellosos (véase Fig. 4).

Figura 4. Anisotricosis. Elaborado sobre el contenido del artículo de González-Saldivar.
Un halo marronáceo, hundido, en las aberturas foliculares también es frecuente (signo peripilar). Cuando el diagnóstico no es evidente, se deben tomar dos biopsias en sacabocados no menores de 4 mm de diámetro, siempre siguiendo la dirección de la vaina del pelo y profundas dentro de la grasa subcutánea, donde normalmente están los bulbos pilosos en fase anágena.
El lugar preferido para la biopsia es el cuero cabelludo central. La biopsia nunca se debe tomar de la zona bitemporal, ya que pueden existir pelos en miniatura independientemente de la AAG [46, 47]. La histopatología muestra el reemplazo de los pelos terminales por vellos secundarios, así como el aumento de la proporción de pelos telógenos sobre los anágenos.
Las recomendaciones generales para el tratamiento de la AAG son la alimentación adecuada, evitar los productos para el cuidado del pelo que podrían empeorar el proceso, suspender los medicamentos que podrían afectar negativamente el crecimiento del pelo (por ej. retinoides, citotóxicos, anticoagulantes) y tratar toda enfermedad de base local o sistémica (por ej. hipotiroidismo, anemia, dermatitis seborreica, psoriasis) [47, 51, 56].
El tratamiento médico es con finasteride o dutasteride por vía oral y minoxidil tópico al 2% y al 5%, que se debe emplear por lo menos durante un año antes de descartar su eficacia. Las operaciones de recuperación del pelo son el trasplante capilar, la cirugía de reducción del cuero cabelludo o una combinación de ambas [47, 59]. La AAG produce estrés psicológico moderado en la mayoría de los hombres y para algunos significa disminución de su calidad de vida [60].
► Hirsutismo, acné e irregularidades menstruales
El síndrome de ovario poliquístico (SOPQ) es una entidad metabólica y reproductiva que aumenta el riesgo de sufrir DT2 y esterilidad [61]. Además de obesidad, las mujeres con SOPQ tienen resistencia a la insulina. La frecuencia de la obesidad es del 25%-70% y contribuye a la resistencia a la insulina [63]. El hiperandrogenismo es una de las características diagnósticas principales del SOPQ y se manifiesta clínicamente como hirsutismo, acné y AAG [65].
El hirsutismo en las mujeres es el exceso de pelo corporal terminal con distribución masculina, en el abdomen inferior , la línea alba, la zona periareolar, el mentón y el labio superior. Afecta al 5% - 10% de las mujeres premenopáusicas y la mayoría de los casos son secundarios al SOPQ [66]. La actividad de la enzima 5-alfa reductasa está aumentada en los folículos pilosos y es estimulada por los andrógenos, el IGF y la insulina para convertir la testosterona a dihidrotestosterona, estimulando el crecimiento capilar [65].
Los diagnósticos diferenciales incluyen, entre otros, la hipertricosis, medicamentos como los glucocorticoides o la ciclosporina, la hiperplasia suprarrenal congénita, el síndrome de Cushing, los tumores secretores de andrógenos y la disfunción tiroidea [68]. El tratamiento comprende modificaciones de los hábitos de vida (hábitos alimentarios, ejercicio y descenso de peso) y tratamientos mecánicos y médicos [69]. El empleo de blanqueadores, la afeitada, la depilación con cera y la depilación con láser son útiles, pero pueden ser dolorosos y caros.
El tratamiento médico comprende los anticonceptivos orales, los agonistas de la hormona liberadora de gonadotropina, los fármacos que sensibilizan a la insulina, como la metformina o los que tienen efectos antiandrogénicos, como el acetato de ciproterona, la eflornitina y la espironolactona [69, 70].
El acné es otra característica de la resistencia a la insulina-hiperandrogenemia en el SPQO y coexiste en el 15–25% de las mujeres con SPQO [71]. Las pacientes con acné con frecuencia tienen aumento de la glucemia y de la insulina, así como resistencia a la insulina [72].
En pacientes con acné vulgar, la desnutrina, también llamada lipasa adiposa de triglicéridos, está baja y se relaciona con los valores de insulina y HOMA-IR [73].
El aspecto del acné es el de lesiones inflamatorias en la zona mandibular, el cuello, el pecho y la parte superior de la espalda. El tratamiento consiste en cambios de los hábitos de vida, como la nutrición y el ejercicio. Se demostró que un pequeño descenso de peso (2–5%) es beneficioso [75, 76].
El tratamiento tópico es con retinoides y benzoil peróxido. Otros tratamientos son sistémicos, con anticonceptivos orales (acetato de ciproterona o drospirenona), espironolactona y antibióticos (minociclina, doxiciclina, azitromicina) y en determinados casos resistentes, isotretinoína [76].
CONCLUSIÓN
La resistencia a la insulina es una característica bioquímica patognomónica de la obesidad y la diabetes. Es uno de los mecanismos de base fisiopatológicos de la diabetes y aparece años antes de su diagnóstico. El diagnóstico preciso de la resistencia a la insulina es complejo e invasivo. Las mediciones y los índices de laboratorio son imprecisos y poco fiables.
Las manifestaciones cutáneas de la resistencia a la insulina, en cambio, ofrecen una manera fiable y fácil de detectarla. Los médicos siempre deben recordar que los trastornos cutáneos de la resistencia a la insulina podrían reflejar un desequilibrio metabólico subyacente que pone al paciente en riesgo de sufrir diabetes si es que ya no la padece. Al mismo tiempo, los profesionales no sólo los deben reconocer, sino evaluar el estado metabólico del paciente y, de ser necesario, aconsejarle con respecto a cambios en sus hábitos de vida, como alimentación saludable, ejercicio, evitar el tabaquismo y descenso de peso.
Resumen y comentario objetivo: Dr. Ricardo Ferreira