|
Resumen • La postura decidida y de avanzada acerca de la cirugía de urgencia continúa siendo el principio rector en el tratamiento inicial de los traumatismos graves. • Algunas intervenciones son mecánicas (torniquetes), otras son farmacológicas (tratamiento antifibrinolítico) y otras exigen nuevas maneras de pensar (cirugía temprana de control de daños). • Desde el primer momento de la lesión, el objetivo debe ser lograr la detención quirúrgica de la hemorragia. • La cirugía de reducción de daños es una estrategia técnica que prioriza la detención de la hemorragia, deja la cavidad abdominal con un cierre temporario y posterga todas las demás maniobras y reconstrucciones quirúrgicas para operaciones ulteriores. • La mayoría de las muertes debidas a hemorragia masiva se producen dentro de los 30 minutos de ocurrida la lesión por lo tanto las intervenciones deben ser inmediatas. • Los pacientes normotensos no deben recibir reanimación con líquidos. • En pacientes hipotensos se debe esperar hasta que la presión sistólica se aproxime a 80 mm Hg. • Los hemoderivados, especialmente cuando se efectúa una transfusión masiva, se deben emplear en todas las instituciones que reciben pacientes con traumatismos. • La reanimación con balón endovascular aórtico (REBOA por las siglas del inglés) es una técnica que está surgiendo rápidamente para detener la hemorragia intracavitaria infradiafragmática no comprimible. |
| Introducción |
Hipócrates escribió, “El que desea ser cirujano debería ir a la guerra”. Es lamentable que el rápido progreso en la asistencia de los traumatismos con frecuencia esté fuertemente vinculado con los conflictos armados. William Mayo, muchos siglos después afirmó, “La medicina es la única vencedora en la guerra.”
Las lesiones provocadas por la guerra a menudo generaron innovaciones en la asistencia de los traumatismos y en la creatividad quirúrgica .Otras evolucionaron a través del camino natural de la revisión externa por expertos, la publicación y aceptación por los colegas. Investigar sobre el tratamiento de las lesiones graves es muy difícil y las innovaciones con frecuencia son impulsadas por la necesidad más que por el método científico.
Sin embargo, las tasas actuales de supervivencia tras un traumatismo grave son las más altas de toda la historia de la medicina y las mejoras recientes en la asistencia médica son atribuibles en parte a las casi dos décadas de guerra contra el terrorismo.
En los Estados Unidos los traumatismos siguen siendo la causa principal de muerte entre las personas de 1-44 años, destacando así que no son solo un problema propio de las guerras.
Este artículo repasa los principales adelantos en la asistencia de los pacientes con traumatismos graves. Practicar la mejor medicina basada en la evidencia para la atención de los traumatismos a menudo exige decisiones imperfectas basadas sobre información incompleta y en evolución. La postura decidida y de avanzada acerca de la cirugía de urgencia continúa siendo el principio rector.
| Torniquetes |
Al inicio de la guerra contra el terrorismo, la tasa de muerte por desangramiento de loa miembros y heridas a nivel de las articulaciones era altísima, a pesar de un informe de 1996 sobre medicina militar donde los autores reconocían la necesidad de emplear torniquetes en terreno para las hemorragias potencialmente mortales de las extremidades. Los torniquetes improvisados fueron frecuentes, aunque muy ineficaces.
Los militares reconocieron la necesidad de un mejor control de la hemorragia de los miembros en el lugar de la lesión y los dispositivos comerciales para detener el desangramiento de los miembros se volvieron comunes en el campo de batalla, junto con la capacitación universal sobre cómo usarlos. Estos cambios redujeron mucho las muertes por desangramiento de las extremidades.
En guerras anteriores los torniquetes cayeron en el descrédito debido al retraso en la evacuación y la pérdida consiguiente de los miembros debido a isquemia. En cambio en los conflictos actuales los tiempos de evacuación son mucho más cortos y esta complicación es rara. También aparecieron vendajes hemostáticos tópicos para evitar el desangramiento de los miembros y articulaciones.
Al regreso de los soldados del frente, los torniquetes comerciales, junto con la capacitación adecuada para su empleo, se popularizaron para las heridas comunes, estimuladas en parte por incidentes con muertes múltiples. Estos episodios terribles alertaron sobre la necesidad de detener rápidamente la hemorragia de las extremidades.
Los datos disponibles indican que todos los servicios de urgencia deberían adoptar esta estrategia intensiva para mitigar la hemorragia en el lugar de la lesión. Una vez aplicado, el torniquete debe seguir ajustado hasta que sea seguro quitarlo para evaluar al paciente en un hospital con capacidad quirúrgica.
| Tratamiento antifibrinolítico |
Aunque la coagulopatía de los traumatismos no se conoce por completo, se sabe que uno de sus componentes es la hiperfibrinólisis maligna. La fibrinólisis es un proceso intravascular normal que mantiene el equilibrio apropiado con la trombosis.
Tras una lesión grave, en algunos pacientes se desarrolla un estado hiperfibrinolítico, donde el trombo es lisado endógenamente con mayor rapidez de la que se puede formar. Esta alteración puede agravar la hemorragia y contribuir a la muerte.
El ácido tranexámico, un fármaco antifibrinolítico, se empleó durante décadas para mitigar la hemorragia posparto. Sin embargo, su utilidad para tratar o prevenir la hiperfibrinólisis en pacientes con traumatismos se reconoció recién pocos años atrás.
El tratamiento con ácido tranexámico es sencillo y su efecto es considerable si se lo da como está indicado en los pacientes con lesiones más graves. (1 g administrado como bolo intravenoso durante 10 minutos, seguido por la infusión de 1 g intravenoso durante 8 horas, administrando la primera dosis dentro de las 3 horas posteriores al traumatismo).
Por estos motivos el ácido tranexámico se adoptó como tratamiento en el campo de batalla y está ganando aceptación en los E.E.U.U. Cuanto antes después del traumatismo se administre el tratamiento, mayor será su utilidad con respecto a las tasas de mortalidad. Se debe ser cuidadoso, sin embargo, ya que la administración de ácido tranexámico más de 3 horas después del traumatismo puede aumentar el riesgo de muerte.
El empleo de este fármaco también se debería incorporar a los programas de transfusión masiva. No se hallaron problemas atribuidos a su adopción universal como intervención inicial para pacientes con sospecha de hemorragia grave.
Aunque no es directamente una intervención antifibrinolítica, la administración de plasma durante el traslado al hospital mejora la coagulación y disminuye la mortalidad global.
| Hipotensión permisiva |
Los pacientes normotensos no deben recibir reanimación con líquidos
Hace un siglo, Walter Cannon afirmó que las fuentes de hemorragia que son inaccesibles o que no se pueden detener no se deben tratar con líquidos intravenosos hasta el momento de la cirugía. Llevó otros 76 años validar esto científicamente en un estudio cuidadoso. Es de lamentar que la estrategia de esperar para la reanimación con líquidos hasta lograr detener la hemorragia se haya difundido lentamente.
Durante la mayor parte del siglo XX, permitir que los pacientes con traumatismos continuaran hipotensos hasta la intervención quirúrgica violaba un principio importante de la reanimación con soluciones de cristaloides. La práctica frecuente de administrar 2 litros de cristaloides en pacientes con traumatismo e hipotensión empeora la coagulopatía y la acidosis y se la debe abandonar.
Los pacientes normotensos no deben recibir reanimación con líquidos, mientras que para esta reanimación en pacientes hipotensos se debe esperar hasta que la presión sistólica se aproxime a 80 mm Hg. En ese momento se deben administrar con cuidado bolos de pequeño volumen de sangre o plasma (250 a 500 ml) a fin de mantener la presión sistólica entre 80 y 90 mm Hg.
Las guerras en Medio Oriente favorecieron el empleo y la aceptación de la hipotensión permisiva. Este enfoque, además de seguro, puede ser muy beneficioso para los pacientes con lesiones penetrantes o romas.
No se sabe cuáles son los límites seguros de la hipotensión permisiva, pero la administración de un gran volumen de líquidos intravenosos antes de la detención quirúrgica de la hemorragia es peligrosa y no se debe efectuar.
| Cirugía de reducción de daños |
La cirugía de reducción de daños es una estrategia técnica para detener la hemorragia masiva.
Este enfoque prioriza la detención de la hemorragia y la reducción de la contaminación en la intervención quirúrgica inicial e implica dejar la cavidad abdominal con un cierre temporario y postergar todas las demás maniobras y reconstrucciones quirúrgicas para operaciones ulteriores.
A veces llamada “cirugía en varios tiempos”, esta intervención favorece la supervivencia en pacientes con las más graves lesiones y las mayores hemorragias. Algunos pacientes deben ser sometidos a operaciones sucesivas durante varios días a fin de evitar el traumatismo de una operación prolongada que implica una amplia hemorragia.
Entre cada operación el paciente estará en la unidad de cuidados intensivos (UCI), donde se lo trata con atención a la reanimación, la resolución de la acidosis, el mantenimiento de la normotermia y la eliminación de la coagulopatía, habitualmente con el empleo de sedación y respiración asistida.
En las operaciones ulteriores se efectúa la reconstrucción quirúrgica definitiva según la tolerancia fisiológica del paciente y se cierra el abdomen en cuanto se completa la reconstrucción. Esta estrategia ha sido adoptada por centros traumatológicos de numerosos países, incluidos aquellos con recursos médicos adecuados.
En la actualidad se la considera la norma asistencial para los pacientes con las más graves lesiones sometidas a cirugía debido a hemorragia masiva. Su empleo atenúa directamente el círculo vicioso de hipotermia, acidosis y coagulopatía.
La operación siguiente se efectuará dentro de las 24 horas de finalizada la primera y cada operación ulterior se deberá efectuar dentro de las 24 horas de la anterior a fin de mejorar las posibilidades de cierre fascial primario. Los intentos quirúrgicos de cierre fascial primario se deben efectuar diariamente, ya que el examen físico no puede pronosticar cuando cerrará la fascia.
El empleo de un dispositivo de vacío para el cierre abdominal temporario y el empleo precoz de bloqueo neuromuscular temporario mejora las tasas de cierre fascial primario y se los debe considerar si no están contraindicados. Los pacientes para la cirugía de reducción de daños se deben seleccionar cuidadosamente, ya que las repetidas operaciones aumentan la morbilidad entre pacientes con lesiones solo moderadas.
| La hora de oro |
Durante la Primera Guerra Mundial los franceses publicaron el primer informe científico sobre la importancia del tiempo en el tratamiento del shock posterior a un traumatismo .El reconocimiento de que la intervención se debe efectuar rápidamente llevó al desarrollo de los sistemas médicos de urgencia.
El apodo “La hora de oro” resumió este enfoque para los encargados de las políticas públicas, si bien pasa por alto la realidad de que la mayoría de las muertes debidas a hemorragia torácica se producen dentro de los 30 minutos de ocurrida la lesión.
Más recientemente, datos de las guerras en Iraq y Afganistán sugieren que la supervivencia en el campo de batalla tras un traumatismo está estrechamente ligada al intervalo entre la lesión y la evacuación para la primera intervención quirúrgica. Esto motivó la orden del Ministerio de Defensa de los E.E.U.U. de evacuar en helicóptero a todos los heridos en combate dentro de los 60 minutos de producida la lesión. Esta orden sirvió para salvar vidas.
Conocer que el traumatismo es sensible al tiempo sigue siendo de la mayor importancia, ya que el intervalo entre traumatismo e intervención quirúrgica determina los resultados, tanto en el campo de batalla como fuera del mismo. La intervención quirúrgica, sin embargo, no se debe confundir con el triage y la reanimación.
Esta última no sustituye a la detención de la hemorragia y se debe ser cauteloso cuando las medidas de reanimación se inician sin un plan para la detención quirúrgica de la hemorragia. El propósito principal del concepto de la hora de oro es conducir todos los esfuerzos hacia la detención temprana de la hemorragia, incluyendo la asistencia inicial, el triage, la evacuación rápida y la reanimación (Figura 1).
Desde el primer momento de la lesión, el objetivo debe ser lograr la detención quirúrgica de la hemorragia. Todas las demás maniobras son de apoyo a este objetivo principal.
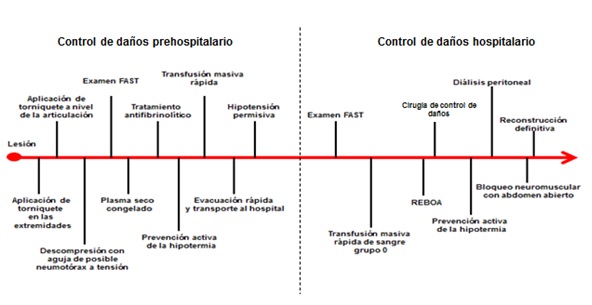
Figura 1. Intervenciones posibles durante la hora de oro
El objetivo principal del concepto de la hora de oro es lograr el control temprano de la hemorragia. Las maniobras prehospitalarias y en el hospital para este objetivo son la asistencia inicial, el triage, la evacuación rápida y la reanimación.
FAST es la ecografía de la cavidad abdominal y el pericardio durante la fase inicial de la asistencia médica.
REBOA es la reanimación con balón endovascular aórtico
|
Los pacientes con hemorragia necesitan sangre. El empleo de otros líquidos intravenosos como medio de reanimación empeora los resultados. La sangre entera o un sustituto parecido a esta se debe emplear para la reanimación, con iniciación simultánea de maniobras de detención de la hemorragia.
Los hemoderivados, especialmente en el contexto de un protocolo organizado de transfusión masiva, con hincapié en una alta proporción de concentrado de eritrocitos: plasma (1:1), se deben emplear en todas las instituciones que reciben pacientes con traumatismos.
Los hemoderivados se refrigeran para su almacenamiento y se deben entibiar a la temperatura corporal a través del uso de un dispositivo de calentamiento de líquidos durante la reanimación. Este es un punto importante porque la transfusión de hemoderivados en un paciente con traumatismo y hemorragia contribuye a la hipotermia y la coagulopatía iatrogénicas.
La velocidad de administración debe ser proporcional al grado de shock y seguir los principios de la hipotensión permisiva. Los hemoderivados se deben administrar a la mayor velocidad posible a fin de respetar los principios de la reanimación hipotensiva, con el objetivo de una presión sistólica de 80 mm Hg durante la cirugía de reducción de daños.
La reanimación no es el sustituto de la detención de la hemorragia. Si se inicia la reanimación se debe iniciar simultáneamente una maniobra de detención de la hemorragia, que incluya, de ser apropiadas, las intervenciones quirúrgicas de reducción de daños.
| Ecografía |
La ecografía de la cavidad abdominal y el pericardio durante la fase inicial de la asistencia médica (FAST por las siglas del inglés de ecografía abdominal focalizada para traumatismos) es tan esencial como la medición de los signos vitales en el triage inicial y las decisiones quirúrgicas, especialmente en el paciente con trauma e hipotensión.
El examen FAST minutos después de la llegada del paciente al hospital es la norma asistencial en la mayoría de los países desarrollados.
El examen FAST ampliado, que incluya también el examen de los espacios pleurales bilaterales, es especialmente útil.
Estas ecografías permiten la detección y la semicuantificación de la hemorragia intraabdominal, que indica la necesidad de cirugía, así como también la detección del hemopericardio traumático (una urgencia médica), el hemotórax y el neumotórax. Esto se puede efectuar rápidamente, momentos después de la llegada del paciente al hospital.
La identificación precoz de estos trastornos permite al médico intervenir inmediatamente o poner en marcha el mecanismo para intervenir con una maniobra para detener la hemorragia, como laparotomía, toracostomía con sonda, o toracotomía sin necesidad de otros estudios radiográficos o de laboratorio.
El lugar del paciente con traumatismo e hipotensión no es la sala de tomografía computarizada y este error frecuente se puede evitar con el empleo del examen FAST a la cabecera del paciente. Otro problema es el resultado falso negativo del examen FAST, que se puede dar incluso en manos experimentadas.
Si el paciente parece sufrir hemorragia abdominal intracavitaria no comprimible, a pesar del FAST negativo, se debe sospechar un examen falso negativo y efectuar otras maniobras diagnósticas como la aspiración o el lavado peritoneal, la toracostomía con sonda bilateral o, en casos apropiados, la laparotomia exploratoria de urgencia.
| Reanimación con balón endovascular aórtico |
Reanimación con balón endovascular aórtico (REBOA por las siglas del inglés) es una técnica que está surgiendo rápidamente para detener la hemorragia intracavitaria infradiafragmática no comprimible. Muchos cirujanos consideran que esta técnica es menos invasiva que la toracotomía de urgencia y el pinzamiento aórtico transversal para el paciente con compromiso hemodinámico, pero sin evidencia de hemorragia torácica y que no se encuentra en paro cardíaco.
El balón de oclusión aórtica se introduce rápidamente en la aorta a través de la arteria femoral común por acceso percutáneo o a cielo abierto, habitualmente durante el triage inicial. El balón se puede entonces colocar en la zona I, proximal al hiato aórtico del diafragma, para detener temporariamente el desangramiento infradiafragmático, después de haber descartado la hemorragia supradiafragmática (Fig. 2).
De lo contrario, el balón se puede colocar en la zona III para detener la hemorragia masiva pélvica o de articulaciones, una vez descartada la hemorragia supradiafragmática e intraabdominal. El principio de descartar la hemorragia en cualquier cavidad proximal a la oclusión con balón es fundamental.
La oclusión distal a una lesión vascular puede acelerar la hemorragia proximal y producir la muerte. Las técnicas para descartar la hemorragia proximal son la ecografía, la radiografía de tórax y pelvis, la toracostomía por sonda diagnóstica y la aspiración o el lavado diagnósticos.
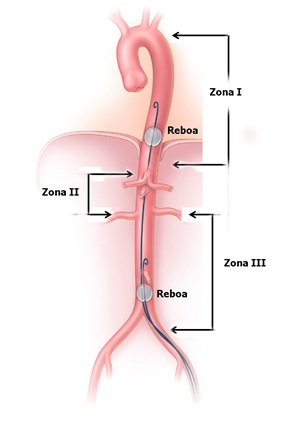
Figura 2. Reanimación con balón endovascular aórtico (REBOA).
Se muestran las zonas de exclusión. En la zona I, se muestra la posición del balón para detener la hemorragia infradiafragmática; en la zona III, se muestra la posición para detener la hemorragia pélvica masiva en ausencia de una fuente abdominal de hemorragia simultánea.
La REBOA permite la detención temporaria de la hemorragia masiva por debajo de la oclusión mientras se efectúa la intervención hemostática definitiva. Esta intervención generalmente es un procedimiento quirúrgico de urgencia (laparotomía) y se elige sobre la base de las características de la lesión: angioembolización pélvica, fijación externa pélvica, empaquetamiento pélvico preperitoneal o la combinación de todas estas intervenciones.
La isquemia visceral abdominal limita el tiempo de oclusión a menos de 30 minutos, pero idealmente este tiempo debería ser lo más breve posible. Técnicas especializadas, como la REBOA intermitente, pueden ser útiles para poder ampliar el tiempo isquémico.
REBOA sigue siendo una intervención con un conjunto de indicaciones, contraindicaciones, técnicas y obstáculos en evolución. Cuando especialistas con experiencia la emplean apropiadamente, REBOA puede mejorar el resultado para el subgrupo de pacientes con las lesiones más graves y las hemorragias más intensas.
Los peligros de REBOA son la isquemia visceral total, la pérdida de miembros inferiores, el empeoramiento de la lesión cerebral traumática, la isquemia de la médula espinal y la hemorragia proximal rápida. Esta intervención, que se emplea con frecuencia en algunos centros de traumatología, merece atención y más investigaciones.
|
Comentario • La atención inicial del paciente con lesiones graves ha cambiado notablemente en las últimas décadas, en gran parte estimulada por la experiencia de las guerras recientes. • Los adelantos continuos en la atención de los traumatismos fuera de los conflictos armados exigen compromiso nacional con la investigación, especialmente en algunos temas con gran promesa, pero pocos datos o aceptación limitada. • La atención de los traumatismos exige un enfoque quirúrgico extremadamente intensivo, pese a la información incompleta, imperfecta y rápidamente cambiante. • Este enfoque se debe emplear inmediatamente, comenzando por el lugar de la lesión. • Es necesario adoptar más ampliamente estos adelantos a fin de mejorar la supervivencia de los pacientes con lesiones más graves, especialmente aquellos con hemorragia masiva. |
Resumen y comentario objetivo: Dr. Ricardo Ferreira