Introducción
La Sociedad de Testigos de Jehová (TJ), fundada en 1872 en Pittsburgh y basada en New York, es una organización religiosa internacional, con alrededor de 7 millones de miembros mundialmente, en más de 230 países [1]. Los TJ generalmente no permiten el uso de productos sanguíneos alogénicos, debido al temor de perder la vida eterna, lo que se basa en la creencia de que la sangre transfundida en un nutriente y que la transfusión de sangre es equiparada con “comer” sangre [2].
Actualmente, sólo los componentes primarios de la sangre (por ej., glóbulos rojos, glóbulos blancos, plaquetas y plasma) están específicamente prohibidos y los componentes secundarios de la sangre, tales como albúmina, crioprecipitados o factores de coagulación, están permitidos, basado en la creencia individual. Adicionalmente, la transfusión de sangre autóloga puede permitirse, si la sangre no es separada del torrente sanguíneo del paciente en ningún momento. No obstante, la donación preoperatoria de sangre con el objetivo de una autotransfusión posterior no es aceptable [1].
El manejo médico de los pacientes TJ genera cuestiones médicas, éticas y legales [3], especialmente en el escenario de procedimientos quirúrgicos mayores, cuando la potencial pérdida de sangre y la necesidad de reemplazo de sangre son significativas. Aunque las tasas de transfusión asociadas con la pancreatectomía y la hepatectomía parcial han disminuido con el paso del tiempo [4-6], esos procedimientos caen aún dentro de la categoría de alto riesgo.
Un número de técnicas de conservación de sangre ha evolucionado, primariamente en respuesta a preocupaciones sobre las complicaciones relacionadas con la transfusión y la declinación del grupo de donantes. El volumen de sangre transfundido está aumentando a una tasa del 6% por año, generando preocupaciones de que la demanda pronto supere a la oferta [7].
El desarrollo de estrategias para la conservación de la sangre, incluyendo la hemodilución aguda normovolémica (HAN), donación de sangre autóloga y el salvataje intraoperatorio de células (CellSaver), han sido importantes para la preservación del suministro nacional de sangre y alguno de esos abordajes puede ser usado en procedimientos quirúrgicos en pacientes TJ.
Los protocolos específicos para la cirugía libre de transfusión han sido desarrollados en algunas especialidades, por ejemplo, en cirugía cardíaca [8]; no obstante, la experiencia con la cirugía del páncreas y del hígado en pacientes TJ es limitada, siendo la mayoría de la literatura existente, reporte de casos [9,10]. Se ha reportado una mayor experiencia en el área del trasplante de hígado sobre el manejo preoperatorio y el uso intraoperatorio de HAN y técnicas de salvataje de células, que parece reducir la necesidad de transfusión [11,12].
El objetivo del presente estudio es revisar la experiencia de los autores con la cirugía para neoplasias del páncreas y del hígado, en pacientes TJ, enfocándose en la seguridad y efectividad de esos procedimientos y de las técnicas perioperatorias usadas.
Métodos
Selección de pacientes y datos registrados
Los datos sobre los pacientes que fueron sometidos a cirugía pancreática y hepática y auto-identificados como TJ, fueron analizados retrospectivamente desde marzo de 1996 hasta julio de 2011. Dos bases de datos prospectivas de operaciones pancreáticas y hepáticas, mantenidas por el Departamento de Cirugía del Memorial Sloan-Kettering Cancer Center (MSKC), así como también las bases de datos institucionales, fueron revisadas para identificar a los pacientes mayores de 18 años de edad sometidos a exploración quirúrgica por tumor hepático o pancreático. Todos los procedimientos quirúrgicos fueron realizados por cirujanos de planta en el Departamento de Cirugía del MSKCC, siendo la indicación primaria la remoción electiva de las neoplasias del páncreas y del hígado.
Los datos preoperatorios analizados incluyeron demografía de los pacientes, antecedentes médicos y quirúrgicos y valores de laboratorio (por ej., hemoglobina, recuento de plaquetas, relación internacional normalizada [RIN], bilirrubina total, albúmina y creatinina). Los datos intraoperatorios fueron obtenidos del protocolo quirúrgico y del registro de anestesia e incluyeron la extensión de la resección, procedimientos mayores concomitantes además del procedimiento principal, duración de la cirugía, tiempo de clampeo porto-hepático (tiempo de Pringle) y pérdida estimada de sangre. Los datos postoperatorios incluyeron duración de la estadía hospitalaria y valores de laboratorio (hemoglobina).
Consentimiento informado preoperatorio
En todos los casos, el cirujano de planta y uno o más anestesiólogos de planta discutieron la operación con el paciente, enfatizando los riesgos asociados con el rechazo a los productos de la sangre, en el escenario de una cirugía mayor y puntualizando las opciones disponibles para la conservación de sangre, incluyendo la optimización preoperatoria de la hemoglobina (mediante hierro y/o eritropoyetina) y el uso intraoperatorio de HAN y el salvataje intraoperatorio de células con el empleo del CellSaver. Se les requirió a todos los pacientes que firmaran un formulario de consentimiento para la realización de procedimientos diagnósticos y terapéuticos sin el uso de productos de la sangre, que describía específicamente los riesgos y abordaba qué opciones de conservación de sangre podían ser usadas.
La técnica de HAN, cuando se la usó, fue aplicada como los autores han descrito previamente para resección del hígado y del páncreas [13,14]. La HAN involucra la remoción de sangre entera del paciente después de la inducción de la anestesia y el reemplazo con cristaloides o coloides, para mantener el volumen intravascular. La sangre removida es luego reinfundida al final del procedimiento. El salvataje de sangre con el uso del CellSaver implica la recolección intraoperatoria de sangre mediante aspiración, filtración y transfusión de vuelta al paciente, con el uso de un equipamiento que mantiene la sangre en circuito con el paciente en todo momento [15]. La eritropoyetina, a menudo combinada con la administración de sulfato de hierro, puede ser usada preoperatoriamente para mejorar la masa de glóbulos rojos, aún en ausencia de anemia [16], aunque este abordaje ha caído recientemente en desgracia debido al aumento del riesgo de trombosis venosa profunda [17].
Técnica quirúrgica
Este estudio analizó sólo a los pacientes que fueron sometidos a hepatectomía parcial o pancreatectomía. Se incluyó a 3 pacientes en los que el intento de hepatectomía o pancreatectomía fue abandonado. Las resecciones hepáticas fueron realizadas con la técnica estándar, usando baja presión venosa central (PVC < 5 cm H2O), principios anestésicos y maniobra selectiva intermitente de Pringle (clampeo porto-hepático), como fuera descrito previamente [5,18].
Después de la operación, los pacientes típicamente fueron monitoreados durante la noche en la sala de recuperación y luego transferidos a la guardia, una vez comprobado que estaban clínicamente estables. Las resecciones pancreáticas fueron realizadas utilizando técnicas estándar, descritas previamente [14,19]. Para la duodenopancreatectomía, el tipo de resección (con preservación del píloro o la resección estándar) fue dictado por la preferencia del cirujano de planta; la reconstrucción fue realizada típicamente con un asa yeyunal mediante una pancreaticoyeyunostomía conducto a mucosa. Los detalles sobre el uso intraoperatorio de HAN y/o salvataje intraoperatorio de células fueron registrados.
Análisis estadístico y registro de complicaciones
El análisis estadístico fue realizado usando el programa SPSS (versión 20.0; SPSS, Inc.). Las variables continuas son mostradas como mediana y rango. Los datos categóricos o dicotómicos son presentados en frecuencias y porcentajes, según lo apropiado.
Las complicaciones postoperatorias fueron registradas prospectivamente en la base de datos de complicaciones del Departamento de Cirugía (MSKCC Surgical Secondary Events Program), para los pacientes admitidos para la operación desde el año 2000 y retrospectivamente, para los pacientes operados antes (n = 6). Todas las complicaciones registradas prospectivamente fueron ingresadas por médicos o personal de enfermería directamente involucrado en la atención del paciente y clasificadas usando un esquema previamente reportado de clasificación de las complicaciones en 5 puntos [20].
Resultados
Datos demográficos y clinicopatológicos
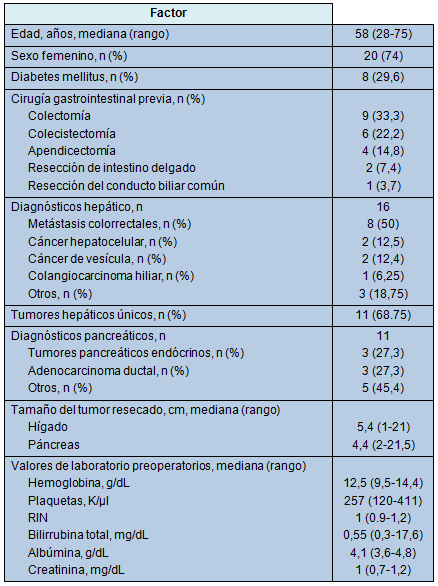
Un total de 27 pacientes sometidos a 28 operaciones (resecciones hepáticas parciales, n = 15; resecciones pancreáticas, n = 10; exploración sin resección, n = 3), entre marzo de 1996 y julio de 2011, fue revisado. La mediana de la edad fue 58 años y 20 pacientes (74%) fueron mujeres. La Tabla 1 resume los datos clinicopatológicos y los datos basales de laboratorio de todos los pacientes. La condición de comorbilidad más frecuente fue la diabetes mellitus en 8 pacientes (29,6%).
El diagnóstico hepático más frecuente fue metástasis de cáncer colorrectal (50%) y los diagnósticos pancreáticos más frecuentes (54,5%) fueron adenocarcinoma ductal y tumores neuroendócrinos. Dos pacientes fueron sometidos a resección hepática por masas hepáticas sintomáticas benignas (adenoma hepático y quiste de hígado). Once pacientes habían recibido quimioterapia antes de la cirugía y todos los 8 pacientes con metástasis colorrectales y 1 con cáncer de vesícula, habían sido sometidos a resección colónica y colecistectomía, respectivamente, antes de la resección hepática.
La mediana del tamaño de los tumores hepáticos resecados fue 5,4 cm (rango, 1 a 21 cm); 5 (31,25%) de los tumores hepáticos fueron múltiples. La mediana del tamaño de los tumores pancreáticos resecados fue de 4,4 cm (rango, 2 a 21,5 cm). Uno de los especímenes hepáticos (6,7%) tuvo evidencias de cirrosis y 4 (26,7%) tuvieron evidencias de esteatosis.
• TABLA 1: Datos demográficos de los pacientes, características del tumor y estudios basales de laboratorio (n = 27)
Evaluación preoperatoria y optimización
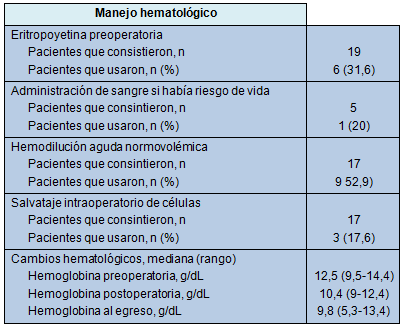
Todos los pacientes firmaron un consentimiento para cirugía libre de transfusión; eventualmente, 4 pacientes consintieron el uso de productos de la sangre en el evento de un sangrado con riesgo de vida. La mayoría de los pacientes consintió el uso de HAN (63%), salvataje intraoperatorio de células (63%) y terapia con eritropoyetina (70,4%). Seis pacientes recibieron eritropoyetina preoperatoria para optimización de la hemoglobina. Los pacientes fueron llevados a la sala de operaciones con una mediana para la hemoglobina de 12,5 g/dL, RIN de 1 y recuentos de plaquetas de 257.000/µL.
Detalles operatorios
La Tabla 2 resume los detalles quirúrgicos de las 28 operaciones. Tres pacientes fueron explorados pero no fueron resecados. En 2 pacientes, las resecciones hepáticas planificadas para metástasis de cáncer colorrectal, fueron abandonadas a causa de enfermedad peritoneal e invasión del tumor del riñón derecho y de la vena cava inferior. El tercer paciente experimentó un sangrado considerable durante un intento de duodenopancreatectomía por un colangiocarcinoma, que fue abandonado debido a compromiso vascular.
• TABLA 2: Detalles operatorios
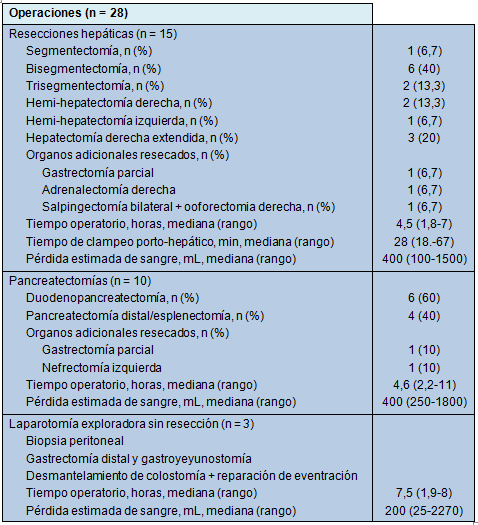
La resección hepática más común fue la bisegmentectomía (40%). La mediana de la duración de la cirugía fue de 4,5 horas (rango, 1,8 a 7 horas) y la mediana de la pérdida de sangre fue de 400 mL (rango, 100 a 1500 mL) La duodenopancreatectomía fue responsable por la mayoría de las resecciones pancreáticas (60%). La mediana de la duración de la operación fue de 4,6 horas (rango, 2,2 a 11 horas) y la mediana de la pérdida de sangre fue de 400 mL (rango, 250 a 1800 mL).
Técnicas de conservación de la sangre
La Tabla 3 resume el manejo hematológico de los pacientes y las técnicas de conservación de la sangre usados. Dos pacientes rechazaron todo uso de eritropoyetina, HAN y salvataje intraoperatorio de células. Cuando fue apropiado, se usó una combinación de técnicas: 1 paciente recibió eritropoyetina preoperatoriamente y HAN y salvataje de células intraoperatoriamente; otros 2 pacientes recibieron eritropoyetina y HAN. Un paciente que había aceptado la transfusión de sangre recibió 2 unidades de glóbulos rojos intraoperatoriamente. La HAN fue usada en un total de 9 pacientes (hígado, n = 5; páncreas, n = 4) removiendo un total de 1 a 4 unidades de sangre entera.
Aunque el sistema CellSaver fue preparado para todos los pacientes que consintieron su uso (n = 17), sólo 3 pacientes tuvieron una pérdida suficiente de sangre para permitir la autotransfusión generada por el CellSaver. Dos de esos pacientes fueron sometidos a hemi-hepatectomía derecha con una pérdida estimada de 1500 mL y 500 mL, respectivamente y el retorno de sangre fue de 225 mL y 125 mL, respectivamente. El tercer paciente con un intento de duodenopancreatectomía que fue abandonado debido a sangrado intraoperatorio, fue sometido a HAN con el uso de 2 unidades de sangre entera y autotransfusión de 405 mL, para una pérdida estimada de 2270 mL.
• TABLA 3: Manejo hematológico
Curso postoperatorio
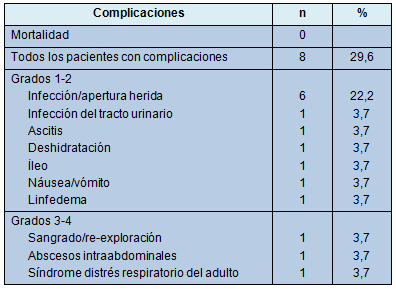
La Tabla 4 ilustra las complicaciones experimentadas. Un paciente requirió re-exploración por descenso de la hemoglobina y rechazo de transfusión, 1 día después de una pancreatectomía distal con esplenectomía, por un tumor pancreático neuroendócrino. Una infección de la herida y absceso abdominal se desarrolló en el mismo paciente. El absceso fue drenado bajo guía tomográfica. Once complicaciones se desarrollaron en otros 7 pacientes (5 infección/apertura, 1 infección del tracto urinario, 1 íleo, 1 náusea/vómito, 1 linfedema, 1 ascitis y 1 síndrome de distrés respiratorio del adulto [SDRA])
La mediana de la estadía hospitalaria fue de 7 días (rango, 4 a 23 días). No hubo muertes postoperatorias dentro de los 90 días para 25 de los 27 pacientes que tuvieron un seguimiento adecuado. La mediana del seguimiento alejado para esa cohorte fue de 22,5 meses (rango, 0,1 a 169 meses), durante el cual 12 de 27 pacientes permanecieron vivos. Las causas de muerte estuvieron relacionadas con el cáncer (46,7%) o fueron desconocidas (53,3%).
• TABLA 4: Complicaciones en 27 pacientes
Discusión
El rechazo a los productos de la sangre en los pacientes TJ, aun con riesgo de lesión orgánica o muerte, tiene sus bases en creencias religiosas que prohíben el “consumo” de sangre [1]. Eso crea desafíos únicos en su manejo, en el escenario de procedimientos quirúrgicos mayores, asociados con la pérdida potencial de sangre, tales como la resección pancreática y hepática. Al mismo tiempo, aunque los componentes primarios de la sangre no están específicamente permitidos, una variedad de otros productos y técnicas puede ser usada, de acuerdo con la interpretación que cada paciente hace de los pasajes bíblicos que conforman el fundamento de su práctica religiosa. La presente serie subraya la variabilidad paciente a paciente en la permisión de las técnicas de conservación de la sangre y la necesidad de una clarificación precisa en cada caso.
Las últimas 2 décadas han visto un considerable progreso en la seguridad de la cirugía del hígado y del páncreas, con reducción sustancial de la necesidad de transfusión de productos de la sangre. A pesar de esas mejoras, sin embargo, esos procedimientos están aún asociados con el potencial para una considerable pérdida de sangre y la potencial necesidad de transfusión de productos sanguíneos alogénicos [5,6].
Una variedad de técnicas, incluyendo PVC baja (< 5 cm H2O) [4], manejo anestésico, uso de clampeo porta-hepático [21] en la cirugía del hígado, uso intraoperatorio de HAN [13] y salvataje de células [22] y uso preoperatorio de eritropoyetina [23] o drogas antifibrinolíticas [24], se han asociado con una declinación de las transfusiones perioperatorias.
El uso objetivo de concentrados de factores de la coagulación podría contribuir también a una reducción adicional en la tasa de transfusión {25]. Aún con la aplicación de esas técnicas, una proporción considerable de pacientes sometida a resección hepática [5,26-28] y pancreática [6,29], en centros de referencia con alto volumen de casos, requiere productos de la sangre. La realización de cirugía del páncreas y del hígado en pacientes TJ sigue siendo desafiante.
Las principales modalidades intraoperatorias usadas para conservar sangre en este estudio fueron las técnicas autólogas de HAN y salvataje de células (CellSaver). Esas técnicas han sido usadas también exitosamente en pacientes TJ en el escenario de trasplante hepático y hepatectomías en donantes vivos [11,12]. La recolección de sangre en la HAN se efectúa después de la inducción anestésica y antes de la parte de resección del procedimiento.
La sangre recolectada es reemplazada con líquidos coloides y/o cristaloides para mantener el volumen intravascular y está disponible para transfusión, si se la necesitara. Por lo tanto, la pérdida de sangre durante la cirugía y en el período postoperatorio resulta en una menor pérdida de glóbulos rojos. Los autores de este trabajo han reportado previamente su experiencia con la HAN en dos ensayos controlados randomizados, mostrando una reducción en la tasa de transfusión para las resecciones hepáticas, pero sin mejoría en los pacientes derivados para duodenopancreatectomía, comparado con el manejo estándar intraoperatorio [13,14].
La HAN es una técnica segura y los pacientes TJ representan un grupo que puede potencialmente beneficiarse con su aplicación. El uso del CellSaver podría ser aceptable para algunos pacientes TJ si la sangre no es almacenada y el circuito está diseñado de manera que permanece en continuidad con la propia circulación del paciente. Representa una técnica segura y efectiva [15]. Se han originado preocupaciones en los pacientes sometidos a cirugía por cáncer, sobre si están en riesgo de diseminación de células cancerosas desprendidas. Sin embargo, recientemente, un meta-análisis de los estudios existentes sobre salvataje intraoperatorio de sangre, no ha mostrado tasas más altas de recidiva [30].
En este estudio no hubo mortalidad perioperatoria y la morbilidad del 25% es aceptable, lo que demuestra la seguridad y factibilidad de la cirugía hepática y pancreática en pacientes TJ. En el presente estudio, la mediana de la pérdida de sangre fue de 400 mL, para las resecciones tanto pancreáticas como hepáticas, algo más baja que los valores medios en series históricas y que refleja, probablemente, una cuidadosa selección de pacientes.
La mediana de la duración de la cirugía fue de 4,5 horas para las resecciones hepáticas y 4,6 horas para las pancreáticas, levemente más largas – por el otro lado – comparadas con los valores históricos de los propios autores para resecciones hepáticas no seleccionadas [5] y resecciones pancreáticas [31]. La optimización preoperatoria de la hemoglobina y la HAN fueron usadas en aproximadamente un tercio y la mitad de los pacientes, respectivamente, que consintieron su empleo.
En contraste, el salvataje intraoperatorio de células, aunque preparado y disponible para la mayoría de los pacientes, resultó en autotransfusión sólo en 3 pacientes con la suficiente pérdida hemática. No queda en claro porqué la HAN y la eritropoyetina no fueron usadas en una proporción más alta de pacientes, pero podría reflejar preocupaciones sobre la complicación trombótica con esta última [17] y la falta de familiaridad con la primera. A pesar del bajo rédito por paciente del CellSaver, representa una importante red de seguridad en el evento de que una hemorragia no esperada y significativa sea encontrada en el curso del procedimiento.
No puede ser suficientemente enfatizado que, aún con la mejora hematológica preoperatoria óptima y la aplicación intraoperatoria de técnicas para la conservación de sangre, se debe mantener un umbral muy bajo para abandonar una operación riesgosa a causa de tumores localmente avanzados involucrando vasos mayores, como ocurrió en 2 pacientes en esta serie, en ambos se produjo una pérdida sustancial de sangre en las primeras etapas de los procedimientos y se determinó que era probable una hemorragia adicional y que las técnicas de conservación de sangre in situ serían insuficientes.
En ese escenario, es imperativo para el cirujano pecar de cauteloso y abandonar el procedimiento, en vez de proseguirlo hasta su conclusión. La selección apropiada de pacientes y la consideración de las variables del paciente y de la enfermedad y el nivel de experiencia y comodidad del cirujano con el procedimiento, se vuelven más críticos que nunca, pero no pueden dar cuenta de todas las situaciones que podrían encontrarse en la sala de operaciones.
La estrategia de evitar las transfusiones de sangre no se debe limitar a los pacientes TJ, sino que deberían ser parte de la práctica quirúrgica de rutina, dado que las transfusiones de sangre se asocian con potenciales efectos colaterales sustanciales [32,33]. El riesgo de transmisión viral o bacteriana, reacciones inmunológicas y aumento de la morbilidad y mortalidad postoperatorias, son sólo algunas de las consecuencias adversas de las transfusiones alogénicas [32,34]. En pacientes con cáncer sometidos a cirugía, la administración de productos de la sangre puede asociarse con recidiva del cáncer y aumento de la mortalidad relacionada con el mismo.
Conclusiones
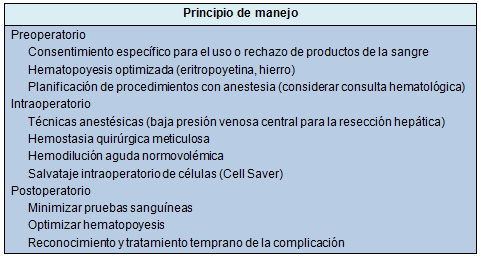
El abordaje interdisciplinario multimodal lleva a excelentes resultados en pacientes TJ después de la cirugía del páncreas y del hígado. La optimización preoperatoria de la hemoglobina, combinada con las estrategias para la conservación intraoperatoria de sangre, una técnica meticulosa para minimizar la pérdida hemática y una atención postoperatoria vigilante, representan los principios para el manejo de los pacientes TJ (Tabla 5), que permiten la realización de resecciones hepáticas y pancreáticas mayores con buenos resultados.
• TABLA 5: Principios para el manejo en pacientes Testigos de Jehová para cirugía hepática y pancreática
♦ Comentario y resumen objetivo: Dr. Rodolfo D. Altrudi