![]()
Introducción
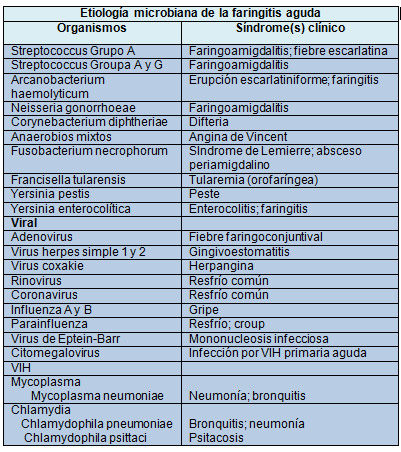
Streptococcus grupo A (SGA) es la causa bacteriana más común de la faringitis aguda, responsable del 5 al 15% de las consultas por dolor de garganta en los adultos y del 20 al 30% en los niños. El diagnóstico seguro de faringitis estreptocócica (faringitis SGA) seguido de un tratamiento antimicrobiano apropiado es importante para: prevenir la fiebre reumática aguda y las complicaciones supurativas (abscesos periamigdalinos, linfadenitis cervical, mastoiditis y, posiblemente, otras infecciones invasivas; mejorar los síntomas y signos clínicos; conseguir la disminución rápida de la propagación del germen; reducir la transmisión de SGA a los miembros de la familia, compañeros de clase y otros contactos cercanos del paciente; permitir la reasunción rápida de las actividades habituales y, minimizar los efectos adversos potenciales del tratamiento antimicrobiano apropiado. Aunque la faringitis aguda es una de las enfermedades más frecuentes para los pediatras y otros médicos de atención primaria, solo un porcentaje relativamente pequeño de pacientes con faringitis aguda (20-30% de los niños y menor porcentaje entre los adultos) sufre faringitis SGA En general, los signos y síntomas de SGA y faringitis no estreptocócica se superponen tanto que por lo general es imposible hacer el diagnóstico solamente sobre la base de los hallazgos clínicos.
Con excepción de muy raras infecciones ocasionadas por ciertas bacterias patógenas faríngeas (por ej., Corynebacterium diphteriae y Neisseria gonorrhoeae), los antimicrobianos no brindan beneficios terapéuticos para la faringitis aguda por organismos diferentes del SGA. Por lo tanto, es extremadamente importante que los médicos excluyan el diagnóstico de faringitis SGA para evitar la administración inapropiada de antimicrobianos a un gran número de pacientes con faringitis no estreptocócica. Dicho tratamiento expone sin necesidad a los pacientes a los costos y los peligros de los antimicrobianos. A pesar de haber mejorado la prescripción para los niños y los adultos con faringitis aguda, un importante número de pacientes continúa recibiendo antibióticos innecesariamente. Este tratamiento innecesario indicado para las infecciones del tracto respiratorio superior, incluyendo la faringitis aguda, ha sido lo que más ha contribuido al desarrollo de la resistencia a los antibióticos de los patógenos comunes. Además de ser una enfermedad aguda, la faringitis SGA es importante porque puede provocar los trastornos post infecciosos no supurativos de la fiebre reumática, con o sin carditis, como así la glomerulonefritis pos estreptocócica. Aunque actualmente la fiebre reumática aguda es infrecuente en los países desarrollados, sigue siendo la causa principal de cardiopatía adquirida en los niños de zonas como India, África subsahariana y regiones de Australia y Nueva Zelanda.
Es importante tener en cuenta que las recomendaciones no siempre pueden explicar las variaciones individuales ni pretende suplantar el criterio médico con respecto a pacientes particulares o situaciones clínicas especiales. La IDSA considera que el cumplimiento de las pautas es voluntario y que la aplicación de las mismas por parte del médico se hará teniendo en cuenta las circunstancias individuales de cada paciente.
El Panel de la IDSA siguió un proceso usado para desarrollar otras guías, clasificando la fortaleza de las recomendaciones (“fuerte”, “débil”) y la calidad de la evidencia (“elevada”, “moderada”, “baja”, “muy baja”) y aplicó el sistema GRADE (Grados de recomendación, Desarrollo y Evaluación). La guía se desarrolló sobre la base de las respuestas a las siguientes preguntas:
| I. ¿Cómo se establece el diagnóstico de faringitis SGA?
II. ¿Quién debe someterse a las pruebas para la faringitis SGA? III. ¿Cuáles son las recomendaciones terapéuticas para los pacientes con diagnóstico de faringitis SGA? IV. ¿Se debe agregar AINE, acetaminofeno, aspirina o corticosteroides al tratamiento específico de los pacientes con faringitis SGA? V. ¿Es posible que el paciente con episodios frecuentes de recurrencia de faringitis SGA sea un portador faríngeo crónico de SGA? |
I ¿Cómo se establece el diagnóstico de faringitis SGA?
1. Hacer el hisopado de fauces y confirmar la faringitis SGA mediante el test de detección rápida del antígeno (TDRA) y/o el cultivo, porque las manifestaciones clínicas no permiten distinguir con certeza la faringitis viral de la estreptocócica, excepto cuando existe rinorrea, tos, úlceras orales y/o dolor de garganta, como sucede en los cuadros virales manifiestos. En los niños y adolescentes, la negatividad del antígeno debe ser confirmada mediante el cultivo del material obtenido mediante el hisopado de fauces (fuerte, elevado). La positividad del TDRA no necesita ser confirmada por el cultivo porque es altamente específica (fuerte, elevado).
2. No es necesario el uso sistemático del cultivo confirmatorio para los pacientes con TDRA negativo o los adultos en circunstancias habituales, debido a la baja incidencia de faringitis SGA en los adultos. Por otra parte, el riesgo de fiebre reumática en los adultos con faringitis SGA es muy excepcional (fuerte, moderado). Los médicos que desean estar seguros de alcanzar la máxima sensibilidad diagnóstica pueden continuar usando el cultivo de fauces convencional o confirmar el TDRA negativo con un cultivo.
3. No se recomienda medir el título de anticuerpos antiestreptocócicos para el diagnóstico de rutina de la faringitis aguda, ya que refleja los eventos pasados y no los actuales (fuerte, elevado).
Características clínicas y epidemiológicos que indican la faringitis estreptocócica Grupo A y la faringitis viral
|
Estreptococo Grupo A ••Inicio repentino de dolor de garganta |
|
VIRAL • Conjuntivitis |
Resumen de la evidencia
La enfermedad se presenta principalmente en niños de 5-15 años, en climas templados y comúnmente ocurre en invierno y el comienzo de la primavera. Los pacientes con faringitis SGA suelen presentar dolor de garganta (en general de comienzo súbito), odinofagia y fiebre. También puede haber cefalea, náuseas, vómitos y dolor abdominal, especialmente en los niños. La semiología muestra eritema faríngeoamigdalino con o sin exudados, a menudo con dolor y agrandamiento de los ganglios linfáticos cervicales anteriores (linfadenitis). Otros hallazgos pueden incluir la hinchazón y el enrojecimiento de la úvula, petequias en el paladar; narinas excoriadas (especialmente en niños) y erupción escarlatiniforme. Sin embargo, ninguno de estos hallazgos es específico de la faringitis GAS. A la inversa, la ausencia de fiebre o la presencia de características clínicas tales como conjuntivitis, tos, ronquera, coriza, estomatitis anterior, lesiones ulcerosas leves en la cavidad bucal, exantema viral y diarrea sugieren fuertemente una etiología viral y no una infección estreptocócica.
II. ¿Quién debe someterse a las pruebas para la faringitis SGA?
4. En general, las pruebas para la faringitis SGA no están recomendadas para los niños o los adultos con faringitis aguda con cuadros clínicos o epidemiológicos que sugieren fuertemente un cuadro viral (por ej., tos, rinorrea, dolor de garganta o úlceras orales) (fuerte, elevado).
5. Los estudios diagnósticos para la faringitis SGA no están indicados para los niños <3 años debido a que la fiebre reumática es rara en esos niños mientras que la incidencia de faringitis estreptocócica y su presentación clásica son infrecuentes. Puede considerarse la realización de estudios en algunos niños <3 años que presentan factores de riesgo, como tener un hermano con faringitis SGA.
Resumen de la evidencia
El SGA como causa de faringitis es más comúnmente observado en niños de 5-15 años, en climas templados, en el invierno y principios de la primavera. Muchos estudios han demostrado que los sistemas de puntaje clínico pueden ser útiles para predecir la probabilidad de infección por estreptococos, pero que la confirmación de laboratorio es esencial para hacer un diagnóstico preciso, ya que los médicos suelen sobrestimar la probabilidad de que la causa de la faringitis sea SGA. Un test negativo para SGA es tranquilizador ya que probablemente la causa de la faringitis sea viral. Un resultado negativo también permite que el médico se sienta seguro al evitar el uso de antibióticos. La realización de estudios para el diagnóstico de SGA según las características clínicas no solo aumenta la proporción de resultados positivos de las pruebas, sino que también aumenta la proporción de pacientes con resultados positivos que están realmente infectados y que no son meros portadores de estreptococos.
Debido al aumento general de las tasas de resistencia a los antibióticos, el tratamiento antimicrobiano debe estar indicado solo en los episodios de faringitis SGA confirmados. En la gran mayoría de los niños y adultos con faringitis aguda la etiología es viral y no necesitan tratamiento antibiótico, aun durante los meses pico. Por otra parte, muchos especialistas apoyan la idea de seleccionar bien a los niños que van a ser estudiados mediante un cultivo de fauces para confirmar el diagnóstico, más para evitar la identificación de los portadores que para identificar a los adolescentes con infección aguda. Las pruebas de SGA deben realizarse en pacientes seleccionados con síntomas y signos clínicos sugestivos de SGA. Mientras el tratamiento precoz consigue una curación clínica más rápida en los pacientes con faringitis SGA aguda y disminuye la transmisión de SGA a otros niños, la razón principal para el tratamiento de esta enfermedad autolimitada es prevenir las complicaciones supurativas y no supurativas. En particular, el tratamiento instituido dentro de los 9 días del comienzo de la enfermedad es efectivo para prevenir la fiebre reumática aguda. Sin embargo, el tratamiento de la faringitis no afecta el desarrollo de glomerulonefritis estreptocócica.
Consideraciones especiales para el diagnóstico de faringitis aguda en adultos. El SGA causa solo el 5 al 15% de los casos de faringitis aguda en los adultos. Sin embargo, el riesgo de faringitis SGA aguda en los adultos es mayor para los padres de niños en edad escolar y las personas que están en estrecha relación con los niños. El riesgo de un primer ataque de fiebre reumática aguda es extremadamente bajo en los adultos, aun con un episodio no diagnosticado ni tratado de faringitis SGA. Debido a estas características epidemiológicas, se ha propuesto un algoritmo clínico sin confirmación microbiológica, como una alternativa aceptable para el diagnóstico de infección en los adultos. Un algoritmo de 4 factores aplicado en el departamento de emergencia predice un resultado positivo de SGA en el cultivo de fauces, con una certeza del 32%–56%, dependiendo del número de manifestaciones clínicas presentes requeridas. No obstante, el uso de esta estrategia diagnóstica daría lugar al tratamiento de un número inaceptablemente grande de adultos con faringitis no estreptocócica; este es un resultado indeseable en este grupo etario, el cual tiene una prevalencia baja de faringitis SGA y un riesgo muy bajo de fiebre o carditis reumática. Sin embargo, debido a las características antes mencionadas de la faringitis aguda en adultos, la exclusión del diagnóstico sobre la base de un TDRA negativo sin confirmación por el cultivo de fauces es una alternativa aceptable para el diagnóstico sobre la base del cultivo de fauces. La elevada especificidad que en general tiene el TRDA minimiza el exceso de prescripción de antimicrobianos para el tratamiento en adultos. Este último punto es de particular importancia, teniendo en cuenta algunos datos nacionales que indican que los antibióticos—con frecuencia el antibiótico de amplio espectro más caro—son prescritos en aproximadamente las tres cuartas partes de los adultos que consultan a los médicos de atención primaria por dolor de garganta. Los médicos que desean estar seguros de alcanzar la máxima sensibilidad diagnóstica pueden continuar usando el cultivo de fauces convencional o asegurarse de un resultado negativo del TRDA con un cultivo.
Niños <3 años con faringitis. Se destaca que en estos niños, la infección SGA suele asociarse a fiebre, rinitis mucopurulenta, narinas excoriadas y adenopatías difusas, y que pueden presentar una faringitis exudativa. La faringitis SGA es significativamente más baja en los niños de esta edad y no se recomienda la realización sistemática de estudios para faringitis SGA. También es muy rara la aparición de fiebre reumática, por lo tanto, salvo que el niño esté en riesgo importante (por ej., tener un hermano con faringitis SGA confirmada o estar en un ambiente de tasas elevadas de faringitis SGA ) se justifica hacer los estudios correspondientes.
Recomendaciones
6. No se recomienda el seguimiento del tratamiento con cultivo del hisopado de fauces o la búsqueda de anticuerpo antiestreptocócicos pero puede hacerse en circunstancias especiales (fuerte, elevado).
7. No se recomienda el estudio diagnóstico sistemático o el tratamiento empírico de los contactos hogareños asintomáticos de los pacientes con faringitis SGA (fuerte, elevado).
Resumen de la evidencia
Cuando a un paciente se le prescribe un antibiótico para el tratamiento de la faringitis SGA, la respuesta clínica se alcanza generalmente a las 24-48 horas de tratamiento. Es importante señalar que la faringitis SGA suele ser una enfermedad autolimitada. Incluso sin tratamiento, la fiebre y los síntomas se suelen resolver a los pocos días del inicio de la enfermedad. La persistencia de los síntomas más allá de ese período sugiere que se ha desarrollado una complicación supurativa o que el niño puede ser un portador crónico de SGA (más que sufrir una infección aguda) con una faringitis viral intercurrente adquirida en la comunidad. Por lo tanto, no se recomienda el seguimiento de los cultivos en forma sistemática. Las pruebas de seguimiento después de un curso terapéutico con un antibiótico apropiado se reservarán para aquellos pacientes con un riesgo particularmente elevado de fiebre reumática aguda o que tienen síntomas recurrentes compatibles con la faringitis SGA.
A pesar de la sensibilidad universal de SGA a la penicilina, el 7% -37% de los niños tratados con un antibiótico apropiado para la faringitis SGA tienen un cultivo de fauces positivo para SGA al final del tratamiento. Estos niños son considerados como fracasos bacteriológicos. En la mayoría de las circunstancias, estos niños son realmente portadores de estreptococos y entonces no está indicada la terapia antimicrobiana.
Contactos asintomáticos del hogar
Es frecuente hallar portadores de SGA entre los contactos familiares de los pacientes con faringitis SGA. Hasta un tercio de los hogares incluye uno o más individuos que desarrollan faringitis SGA sintomática, lo que crea la necesidad de realizar pruebas diagnósticas y tratamiento. Los trabajos sobre el papel de la profilaxis antibiótica de los contactos familiares de pacientes con faringitis SGA no han demostrado que la profilaxis con penicilina reduzca la incidencia de faringitis SGA posterior, aunque se ha comprobado un efecto pequeño y estadísticamente significativo por la profilaxis con cefalosporinas. Los antibióticos se han asociado con efectos secundarios adversos (erupción, diarrea y, raramente, anafilaxia) mientras que el uso innecesario de los antibióticos de amplio espectro puede dar lugar a la propagación de microorganismos resistentes a los antibióticos en la población. Dada la naturaleza autolimitada de la faringitis SGA, la elevada frecuencia del transporte de SGA en las fauces, la limitada eficacia de la profilaxis con antibióticos, y los riesgos directos e indirectos potenciales asociados su uso sistemático, no se justifican las pruebas o el tratamiento de rutina en los contactos familiares asintomáticos de los pacientes con faringitis SGA.
Recomendaciones para el manejo de los pacientes con faringitis SGA
III. ¿Cuáles son las recomendaciones terapéuticas para los pacientes con diagnóstico de faringitis SGA?
Recomendaciones
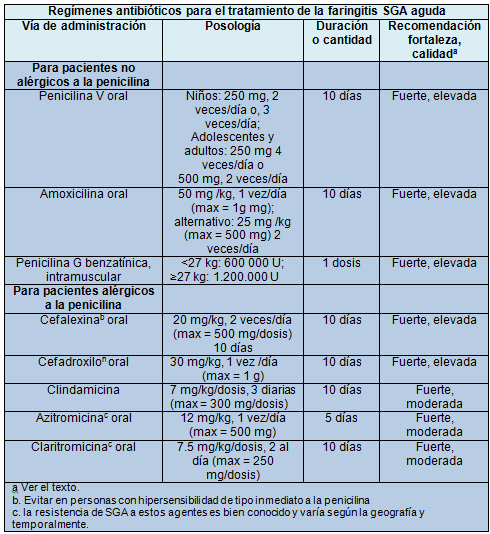
8. Los pacientes con faringitis aguda SGA deben ser tratados con los antibióticos y las dosis apropiados, durante un lapso que erradique al organismo de la faringe (comúnmente 10 días). Debido a su estrecho espectro de efectividad, la poca frecuencia de las reacciones adversas y el bajo costo, la penicilina o la amoxicilina son los antibióticos de elección recomendados para los pacientes no alérgicos a esos agentes (fuerte, elevado).
9. Para el tratamiento de la faringitis SGA de individuos alérgicos a la penicilina se puede prescribir durante 10 días una cefalosporina de primera generación (para pacientes anafilácticamente sensibles), clindamicina o claritromicina durante 10 días o, azitromicina durante 5 días (fuerte, moderado).
Resumen de la evidencia
Al seleccionar un antimicrobiano para el tratamiento de la faringitis SGA, hay que tener en cuenta cuestiones importantes como la eficacia, la seguridad, el espectro antimicrobiano (amplio o estrecho), la posología, el cumplimiento del tratamiento y el costo. Estos factores influyen en el costo-efectividad de la terapia antimicrobiana. Varios antibióticos han demostrado ser eficaces para el tratamiento de la faringitis SGA: la penicilina y sus congéneres (ampicilina, amoxicilina), numerosas cefalosporinas, los macrólidos y la clindamicina. La penicilina, sin embargo, sigue siendo el tratamiento de elección debido a su demostrada eficacia y seguridad, su espectro estrecho, y su bajo costo. Nunca se ha documentado la existencia de SGA resistente a la penicilina. Para los niños pequeños, en lugar de la penicilina a menudo se usa la amoxicilina por vía oral, con igual eficacia. Esta elección se debe principalmente a la aceptación del sabor de la suspensión. Ensayos clínicos comparativos han demostrado que la amoxicilina 1 vez/día, (50 mg/kg, hasta un máximo de 1000 mg) durante 10 días es eficaz para la faringitis SGA. Este agente, de cierto amplio espectro tiene la ventaja de administrarse 1 vez/día, lo que puede mejorar la adherencia, es relativamente barato y de sabor agradable.
La mayoría de los antibióticos orales deben administrarse durante 10 días para alcanzar tasas máximas de erradicación de SGA de la faringe. En la actualidad, la Food and Drug Administration de EE. UU. ha aprobado el cefdinir, la cefpodoxima y la azitromicina durante un curso de 5 días para el tratamiento la faringitis SGA. Sin embargo, faltan estudios de corta duración para establecer criterios estrictos de tratamiento con las cefalosporinas. Por otra parte, el espectro de estos antibióticos es mucho más amplio que el espectro de la penicilina, y, aun cuando se administran durante cursos más cortos, son más caros. Por lo tanto, el uso de estos cursos de cefalosporinas orales más cortos no puede ser aprobado por el momento.
Los antimicrobianos para la faringitis SGA pueden administrarse por vía oral o parenteral. Cuando se considera que el paciente tiene poca probabilidad de completar el tratamiento de 10 días por vía oral, es preferible la penicilina G benzatínica intramuscular. Ciertos antimicrobianos no se recomiendan para el tratamiento de la faringitis SGA, como las tetraciclinas, que tienen una prevalencia elevada de cepas resistentes. Las sulfonamidas y trimetoprima-sulfametoxazol no deben ser utilizados porque no erradican al SGA de los pacientes con faringitis aguda. Las fluoroquinolonas mayores (por ej., la ciprofloxacina) tienen una actividad limitada en la faringitis SGA y no deben ser utilizadas para su tratamiento. Las fluoroquinolonas más nuevas (levofloxacina y moxifloxacina) son activas in vitro contra SGA, pero son caras y tienen un amplio espectro que no se necesita y por lo tanto no se recomiendan para el tratamiento de rutina de la faringitis SGA.
Para la mayoría de los individuos alérgicos a la penicilina se recomienda un curso de 10 días de una cefalosporina oral. Las cefalosporinas de espectro estrecho, como la cefalexina o el cefadroxilo se prefieren a las cefalosporinas de amplio espectro, como el cefaclor, la cefuroxima, la cefixima, el cefdinir y la cefpodoxima. La mayoría de las cefalosporinas orales de amplio espectro son mucho más caras que la penicilina o la amoxicilina, y los agentes más antiguos son más propensos a encontrar resistencia en la flora bacteriana. Algunas personas alérgicas a la penicilina (hasta 10%) también son alérgicas a las cefalosporinas, por lo tanto, estos agentes no deben ser utilizados en los pacientes con hipersensibilidad inmediata a la penicilina (de tipo anafiláctico).
La resistencia a la clindamicina entre los SGA aislados en EE. UU. es de casi el 1%, siendo éste un agente apropiado para el tratamiento de los pacientes alérgicos a la penicilina como así un macrólido (eritromicina o claritromicina) o una azalida oral (azitromicina en una dosis de 12 mg/kg/día, hasta un máximo de 500 mg). Todos los antibióticos se administran durante 10 días menos la azitromicina que se administra durante 5 días.
La eritromicina se asocia a con tasas mucho más elevadas de efectos secundarios gastrointestinales que los otros agentes. Las cepas de SGA resistentes a estos agentes se han hallado muy frecuentemente en algunas zonas del mundo y han dado lugar al fracaso terapéutico. En los últimos años, las tasas de resistencia a los macrólidos halladas en los aislados faríngeos de la mayoría de las zonas de EE. UU. han sido del 5% al 8%. Un estudio sugiere que 10 días de claritromicina puede ser más eficaz para erradicar al SGA en los cuadros de faringitis que 5 días de azitromicina.
Terapéutica adicional para el estreptococo de las fauces
IV. ¿Se debe agregar AINE, acetaminofeno, aspirina o corticosteroides al tratamiento específico de los pacientes con faringitis SGA?
Recomendaciones
10. El tratamiento adicional puede ser útil en la faringitis SGA.
(i). Si se desea, cuando hay síntomas graves o para controlar la fiebre, además del tratamiento antibiótico, se pueden prescribir analgésicos/antipiréticos como los AINE o el acetamonifeno.
(ii). Evitar la aspirina en los niños (fuerte, moderado).
(iii). No se recomienda el agregado de corticosteroides (débil, moderado)
Resumen de la evidencia
Muchos estudios, incluyendo estudios aleatorizados, doble ciego y controlados con placebo, han demostrado el beneficio de los AINE, como el ibuprofeno, para disminuir la fiebre y el dolor, en comparación con el placebo, tanto en niños como en adultos con faringitis, sin efectos adversos importantes. En otro estudio aleatorizado, doble ciego y controlado con placebo se comprobó un gran alivio del dolor con acetaminofeno comparado con placebo, también en niños y adultos, aunque la mejoría de los síntomas no siempre fue equivalente a la obtenida con el ibuprofeno. Aunque la aspirina también ha mostrado su acción analgésica en los adultos con infecciones del tracto respiratorio superior, los autores no recomiendan su uso para el alivio del dolor de la faringitis en los niños, debido al riesgo de síndrome de Reye.
Los resultados de estudios aleatorizados, doble ciego y controlados con placebo demostraron que los corticoides disminuyen la duración y la gravedad de los signos y síntomas de la faringitis SGA en adultos y niños, aunque la disminución real de la duración del dolor es mínima (aproximadamente 5 horas). Es difícil comparar la magnitud del efecto entre varios estudios debido a las diferencias en el agente seleccionado, la vía de administración y la posología utilizada; el método para evaluar el dolor, la duración del seguimiento y las limitaciones del seguimiento por teléfono. El efecto de la administración concomitante de AINE y acetaminofeno en estos pacientes es poco claro. Dada la eficacia de los antimicrobianos, la naturaleza autolimitada de la faringitis SGA, la eficacia de los analgésicos sistémicos y de algunos analgésicos de uso tópico, y el potencial de efectos adversos de los esteroides sistémicos, los autores no recomiendan su uso en esta enfermedad.
En el mercado existen varios agentes tópicos para el tratamiento de la faringitis aguda, como buches, aerosoles y pastillas. Varios contienen anestésicos tópicos, como ambroxol, lidocaína y benzocaína, los que pueden aliviar temporariamente el dolor. Las pastillas pueden ser efectivas pero en los niños pequeños entrañan el peligro de asfixia. No hay trabajos que hayan estudiado en detalle el uso de buches con agua tibia y sal.
V. ¿Es posible que el paciente con episodios recurrentes frecuentes de faringitis SGA sea un portador faríngeo crónico de SGA?
Recomendaciones
11. Los autores recomiendan que los médicos que atienden pacientes con episodios recurrentes de faringitis asociados con pruebas de laboratorio positivas para SGA consideren que pueden experimentar más de 1 episodio de faringitis SGA verdadera a pequeños intervalos, pero también deben tener en cuenta la posibilidad de que el paciente en realidad sea un portador crónico de SGA que experimenta infecciones virales repetidas (fuerte, moderado).
12. Los autores sostienen que los portadores SGA no siempre justifican los esfuerzos para identificarlos ni suelen requerir tratamiento antimicrobiano porque es improbable que contagien a los contactos cercanos y tienen poco o ningún riesgo de desarrollar complicaciones supurativas o no supurativas (por ej., fiebre reumática aguda (fuerte, moderado).
13. No se recomienda la amigdalectomía con el solo fin de reducir la frecuencia de la faringitis SGA (fuerte, elevado).
Resumen de la evidencia
Debido a que no se recomienda volver a hacer las pruebas después de finalizado el tratamiento de la faringitis aguda SGA, las mismas solo se harán en los pacientes con signos y síntomas recurrentes de faringitis aguda ocurrida a las semanas o meses de haber completado el tratamiento de una faringitis aguda. Si estos pacientes sintomáticos vuelven a presentar un cultivo de fauces o un TRDA positivo, se puede deber a diferentes causas: falta de cumplimiento del tratamiento antibiótico; una infección faríngea SGA nueva por un contagio familiar o de compañeros de escuela o de otros contactos de la comunidad o, ser un portador crónica de SGA con infecciones virales intercurrentes. No se puede descartar que el segundo episodio de faringitis esté causado por la cepa de SGA infectante original, pero esta situación es menos común.
Los portadores faríngeos crónicos tienen SGA en la faringe pero no tienen evidencia de una respuesta inmunológica activa contra el organismo, como sería el aumento del título de anticuerpos antiestreptocócicos. Durante el invierno y la primavera en los climas templados, casi el 20% de los escolares asintomáticos puede ser portador de SGA. Estos niños pueden estar colonizados por SGA en la faringe durante ≥6 meses y durante ese tiempo pueden experimentar episodios de faringitis viral recurrente. Las pruebas para estos pacientes suelen mostrar evidencia de SGA en la faringe y por lo tanto pueden semejarse a los pacientes con faringitis SGA aguda. Los individuos identificados como portadores crónicos de SGA en la faringe habitualmente no requieren más tratamiento antibiótico. Es improbable que los portadores diseminen el organismo a sus contactos cercanos y se cree que el riesgo de desarrollar complicaciones supurativas o no supurativas es muy bajo, si es que lo hay.
Por otra parte, es mucho más difícil erradicar la faringitis SGA de las fauces de los portadores que de los pacientes con infecciones agudas SGA. Esto es particularmente cierto para el tratamiento con penicilina o amoxicilina y puede también serlo para otros antimicrobianos. La evidencia clínica y epidemiológica indica que, en estudios publicados que muestran que la penicilina o la amoxicilina tienen tasas relativamente elevadas de falla terapéutica para erradicar la faringitis SGA, la población de pacientes fue probablemente “contaminada” por los portadores crónicos.
El tratamiento antimicrobiano no está indicado en la gran mayoría de portadores crónicos de estreptococos. Sin embargo, hay situaciones especiales en las cuales se puede desear la erradicación del transporte: 1) durante un brote comunitario de fiebre reumática aguda, glomerulonefritis posestreptocócica aguda o infección SGA invasiva, 2) durante un brote de faringitis SGA en una comunidad cerrada o semicerrada, 3) cuando hay antecedentes familiares o personales de fiebre reumática aguda, 4) en una familia con mucha preocupación por las infecciones SGA o, 5) cuando se ha considerado hacer la amigdalectomía solamente porque el individuo es un portador SGA. Se ha demostrado que algunos regímenes antibióticos destinados a erradicar el transporte crónico de estreptococos son más efectivos que la penicilina o la amoxicilina.
En la práctica diaria suele ser difícil diferenciar un portador de SGA con una infección viral intercurrente de un paciente con faringitis SGA aguda. Los datos útiles son la edad, la estación del año, las características epidemiológicas locales (por ej., la prevalencia local de influenza y/o enfermedades enterovirales) y, la naturaleza precisa de los signos y los síntomas.
Sin embargo, en muchos casos, el médico no puede distinguir el transporte persistente de una infección aguda y decidirá administrar otro curso de antibióticos. Para un solo episodio de faringitis que ocurre enseguida de haber completado el tratamiento con un antibiótico apropiado, acompañado con SGA confirmado por el laboratorio, es válido hacer el tratamiento con cualquier agente, como figura en la siguiente tabla.
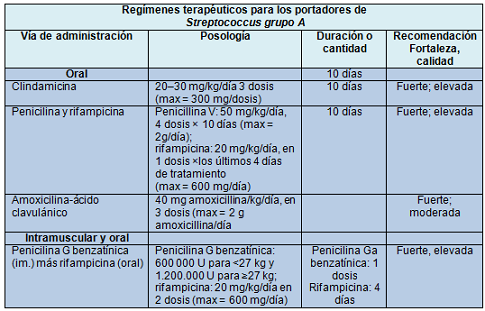
Debido a que la adherencia del paciente al tratamiento antimicrobiano oral suele ser un problema, se puede considerar la administración de penicilina G benzatínica por vía intramuscular. Para esos segundos episodios individuales, luego del segundo curso de antibiótico no es necesario obtener otra muestra del hisopado faríngeo para EL cultivo, a menos que el paciente siga sintomático, o comience a tener síntomas o, presenta al menos alguna de las circunstancias mencionadas antes. Una circunstancia clínica aún más problemática es la persona (usualmente un niño en edad escolar o un adolescente) que, dentro de un período de meses a años experimenta múltiples episodios de faringitis aguda con identificación de SGA en el cultivo y/o el TRDA. Es posible que la mayoría de esos pacientes sean portadores crónicos de estreptococos y experimenten infecciones virales repetidas.
Para los pacientes con episodios aislados frecuentes, es necesario tener en cuenta la naturaleza precisa de la presentación de los signos y síntomas, la respuesta clínica al tratamiento antibiótico y la presencia o ausencia de faringitis SGA en los cultivos del hisopado faríngeo durante los intervalos asintomáticos ayudan a distinguir el transporte persistente de los episodios recurrentes de faringitis SGA aguda. La serotipificación o la genotipificación de los estreptococos aislados de las muestras obtenidas durante los diferentes episodios de un paciente individual también pueden ayudar, porque a lo largo del tiempo en el portador persiste la misma cepa de SGA. Lamentablemente, estos estudios solo están disponibles en laboratorios de investigación especializados y es improbable que lo estén en el marco de la práctica habitual. No se han hecho estudios controlados definitivos del tratamiento de los episodios sintomáticos repetidos múltiples de faringitis aguda con cultivo positivo en la misma persona. Sin embargo, los regímenes establecidos para los portadores crónicos hacen que las tasas de fracaso bacteriológico sean bajas. No se recomienda la profilaxis antimicrobiana continua excepto para prevenir la fiebre reumática aguda recurrente en los pacientes que han experimentado un episodio previo de esa enfermedad.
Si el médico sospecha que los episodios infecciosos recurrentes dentro de una familia se deben a la diseminación “ping-pong”, puede ser útil obtener muestras por hisopado faríngeo de todos los contactos familiares, en forma simultánea, para tratar a los que tienen un resultado positivo en el cultivo o el TRDA. No hay evidencia cierta de que las mascotas de la familia sean reservorios de SGA en la faringe o que contribuyan a la diseminación dentro de la familia.
La amigdalectomía puede ser considerada en ciertos pacientes cuyos episodios sintomáticos no disminuyen en frecuencia a los largo del tiempo y para quienes no se halla una explicación evidente alternativa de la faringitis SGA. Sin embargo, se ha demostrado que beneficia solamente a un grupo relativamente pequeño de estos pacientes y puede ser que cualquier beneficio termine en el corto plazo.
Investigaciones futuras
Las investigaciones futuras deben tener como objetivo:
1) Mejorar los métodos rápidos para el diagnóstico de la faringitis SGA aguda y distinguir la infección aguda del transporte faríngeo crónico del estreptococo,
2) Desarrollar regímenes terapéuticos más simples o cortos para la faringitis SGA aguda.
3) Desarrollar una vacuna asequible, segura y efectiva contra el amplio espectro de organismos SGA.
♦ Traducción y resumen objetivo: Dra. Marta Papponetti
